HPV vaccination campaigns announced in Europe – Time for parents to get informed!
The World Health Organization’s global strategy to accelerate the uptake of HPV vaccination was adopted in August 2020. WHO’s global strategy has the target rate of vaccine uptake defined as 70-90% by 2030. The WHO European Region Roadmap agreed in 2022 aligned with the global objectives, and is now ready for deployment across Europe, both in EU and EEA countries. HPV vaccination is being offered to children and teens with varying recommendations defining the age for vaccination as young as nine.
Diverse campaigns are starting as the school year begins, with enhanced methods incorporating COVID-19 vaccination campaign mastery and results of several bench-marking exercises across the globe. The Implementation Tool developed by the WHO’s Regional Office for Europe or the proposed interventions by the WHO suggest numerous ways to maximize the uptake among young girls and boys through techniques ranging from educational and promotional “nudge” tactics to school-based vaccination clinics. The vaccine in question is Merck’s cash cow, Gardasil 9.
HPV vaccine is said to prevent cervical, vaginal, vulvar and anal cancer, as well as genital warts. However, there is much controversy surrounding the product. The article brought to you here is intended to highlight the crucial facts about this vaccine for consideration.
In line with the World Health Organization’s policies, the two-year project, PROTECT-EUROPE, was launched in January 2023 and is coordinated by the European Cancer Organization under the EU4Health programme 2021-2027 .
PROTECT EUROPE is a project to get more young people in Europe vaccinated by promoting gender-neutral HPV vaccination programs in the European Union (EU) member States.
A recent report published by the European Cancer Organization suggests numerous ways of doing just that.
Several EU member States are already implementing the methods also listed in this report and campaigns are either on-going or expected to be launched this autumn.
The 65-page long report discusses various ways to promote vaccine uptake, such as educational and promotional “nudge” techniques, “time-for-your-vaccine” reminders, incentives (for example gift vouchers) and school-based vaccination clinics.
The vaccine is Gardasil 9 which is indicated as a protection against nine different types of human papilloma virus (HPV). Some HPV infections are associated with certain types of cancer, such as cervical, anal, penile and oropharyngeal cancers. This means that their presence is frequent in those types of cancers, but not necessarily that they are the cause of the disease. While HPV infections are prevalent, these cancers are very rare. The vaccine’s manufacturer, Merck, markets this vaccine for 11–45-year-olds as a way of preventing precancerous lesions and cancers.
The word cancer is an emotionally charged word which instills a lot of fear in most people and understandably so. A parent’s first thought might be something along these lines: “If this vaccine prevents cancer, how can I not vaccinate my child?”
It is important to be fully informed before rushing into any medical intervention. Knowing the facts usually decreases fear and allows us to pause to think and evaluate the situation in a reasonable manner.
For parents to make an informed decision as to whether or not to vaccinate their pre-adolescents of age 11-12, they need to access non-biased and up-to-date material on the following points:
- What is human papilloma virus (HPV)?
HPV is a group of more than 200 related viruses, some of which are spread through vaginal, anal, or oral sex. Most HPV strains cause no disease is the reassuring message one can read on the National Cancer Institute’s web pages. However, some of them are more frequently found in association with cancer than others.
What is the frequency of HPV infections?
On the CDC website it says that HPV infections are very common and that nearly everyone will get HPV at some point in their lives.
Does catching an HPV infection mean that your child will develop cancer?
No, 9 out of 10 – 90% of HPV infections – resolve by themselves within two years.
Among the HPV infections which linger on for longer, a very small percentage of these can evolve into lesions and an even smaller percentage of those lesions can in turn evolve into cancer. This usually takes several years.
Are HPV infections the cause of cervical, penile and anal cancers?
The answer to this question is not as straightforward as we could hope. Cancer is a multifactorial disease with several genetic and environmental factors involved.
There are known environmental risk factors that have been linked to cervical cancer. However, a risk factor should not be considered a cause because the presence of a risk factor will not systematically lead to cancer.
An article published on the National Institute for Health’s PubMed central explains the “multifactorial nature of human papillomavirus persistence and oncogenesis”. Some types of HPV are associated with, for example, cervical cancer and are therefore considered to be one of several risk factors for that disease. Some of the other risk factors for cervical cancer are:
- A poorly functioning immune system (either due to existing disease, medication or lifestyle issues such as poor nutrition and high levels of stress)
- Other genital infections, especially when reoccurring, such as herpes.
- Smoking, which drastically increases the risk for cervical cancer and other cancers.
To conclude, cervical cancer and cancer in general does not have one single cause. It is multifactorial. An HPV infection does not systematically evolve into cancer. Even if the HPV in question has been associated with specific types of cancer, its presence does not necessarily lead to cancer. It constitutes one of several risk factors.
This information is accessible on national and international websites all over the world.
Since some HPVs have been found in association with cervical, anal, penile and oropharyngeal cancers, it is important to find out more about these cancers. This brings us to a second set of questions:
- What is the median age of occurrence of these cancers?
- Are they high incidence cancers?
- Are they treatable?
- Are there ways to prevent these cancers besides vaccination?
- What is the vaccine’s efficacy and safety profile?
With this information on board, it becomes easier to consider the risk-benefit ratio for the Gardasil 9 vaccine.
There are websites dedicated to cancer research and cancer statistics available in most European countries where country-specific statistics can be found.
In France, several websites exist: The National Institute for cancer, La Fondation ARC for cancer research, et InfoCancer – ARCAGY-GINECO, to mention a few.
As far as promoting the HPV vaccine goes, these websites follow the governmental guidelines of their country, which in turn have been influenced by the European Union’s guidelines. They do not tackle the prickly subject of pros and cons, risks and benefits linked to the HPV vaccine.
It would be practically impossible for these organizations to do so; ask questions or be less than enthusiastic when the government and the media take such a firm stance on this topic. They are obliged to follow national guidelines, be they political or medical, and promote the HPV vaccination. Looking to them for a thorough risk and benefit analysis for the Gardasil vaccine is therefore of no use.
However, these websites do contain a lot of data on national and international cancer statistics which is very useful for parents to learn more about the different anogenital cancers.
The numbers for cancer incidence vary slightly between the different European member states. The European Cancer Information System – ECIS – offer comparative numbers for all the countries in Europe. However, the easiest access to country-specific numbers is most likely on national websites.
The following information is taken from the French website, InfoCancer.
Facts about cervical cancer
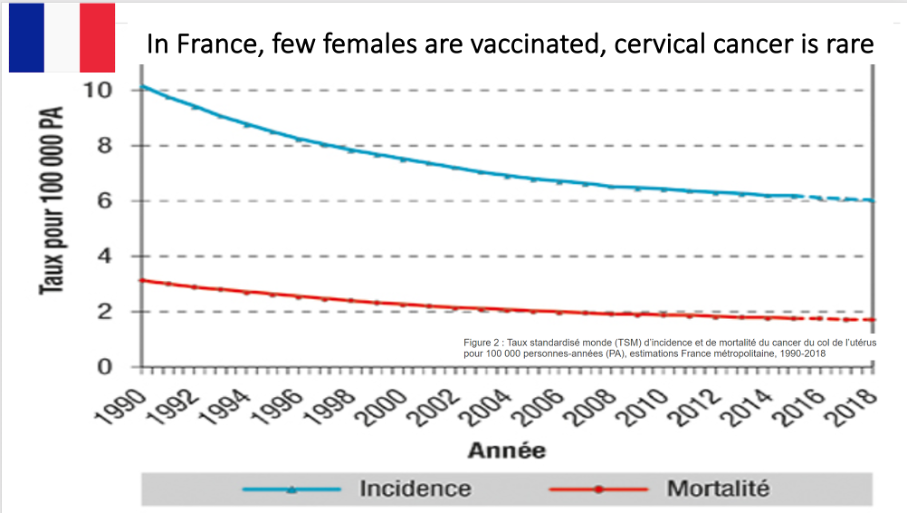
“Its annual incidence per 100,000 women has been falling steadily over the past 20 years. It has fallen from 14.9 in 1980 to 6 in 2018 (-3% per year), and this thanks to organized screening in certain regions, the practice of pap smears and the search for genital infections due to HPV.”
“The disease can occur at any age, although the median age of onset is 53. It is easily detected through regular screening and treatable”.
The incidence and death rates of the disease are much higher in some developing countries, where screening is not available, and the living conditions are very different. The incidence can be as high as 55 out of 100 000 in certain places around the world.
“The risk of developing the disease in a woman’s lifetime is less than 1% in France, and 5% in developing countries”.
Cervical cancer is detectable and treatable with an age standardized relative survival rate at around 70%. For young women between 14 – 44, it is as high as 80%.
In countries like Finland, which have good screening practices, the annual incidence rate is as low as 4 per 100 000 women.
Facts about penile cancers
According to the French InfoCancer website, penile cancers are also low incidence cancers, even lower than cervical cancer:
“In France, the incidence of penile cancer is estimated at 1 case per 100,000 men. It generally occurs in the 60s, peaking at around age 80 (median age 71).”
Facts about anal cancers
“Anal cancers are rare, with a standardized annual incidence of 1 per 100,000 people, which represents around 2,000 new cases per year in France. Two thirds of the patients are over age 65.”
Facts about oropharyngeal cancers
And let’s also look at the oropharyngeal cancers, the cancers of the oropharynx, the middle part of the throat, where an HPV infection can also develop and possibly be associated with cancer at a later stage if not resolved by the body’s immune system.
On the InfoCancer website, these types of cancer are of decreasing incidence. “The standardized incidence rates are 4.8 for men and 0.8 for women, giving a male/female ratio of 6.0. The age of onset is between 50 and 74, with an average age of diagnosis of 71. The two major risk factors involved in these types of cancers are smoking and alcohol with an increased risk of up to 25% for smokers.”
On Merck’s website, it is specified for Gardasil 9 that “The oropharyngeal and head and neck cancer indication is approved under accelerated approval based on effectiveness in preventing HPV-related anogenital disease. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.”
This means that the Gardasil 9’s indication has been extended to include oropharyngeal cancers, maybe only temporarily, because of an assumed effectiveness. Since the HPV vaccine is indicated for prevention of HPV related anogenital disease (cervical and anal cancers), it is assumed that it will also be effective against the oropharyngeal cancers with the presence of HPV. However, this remains to be verified in future clinical trials.
Vaccine efficacy
The cancers associated with certain types of HPV, as we can see from the numbers in France, are low incidence cancers with an average age of onset for some of them as high as 71.
This poses an essential question: How did Merck’s clinical trials determine the efficacy of their vaccine for cancers that could happen 20-30 years or more after vaccination? How can Merck claim that its vaccine will protect 12-year-old children against cancer all the way into their 50s or 60s, the median age of most of these cancers?
It seems extremely difficult if not impossible to verify the efficacy of a vaccine that far into the future. The duration of the clinical trials would have to be extremely long and they would also be incredibly costly with a vaccine put on the market several years from now.
How did Merck get around this?
Dr Michel de Lorgeril is a French physician and international expert in epidemiology and physiology. A graduate of European universities, he joined the French National Center for Scientific Research (CNRS) in 1990. His scientific and medical background makes him a specialist in scientific methodology, particularly for evaluating medical research. He has written numerous books aimed at both the general public and medical professionals including a series of nine books called “Vaccins et société.” This series intends to make scientific papers and clinical studies concerning vaccines more accessible to the general population.
In his book, “Les Vaccins contre les cancers – rôle des Papillomavirus”, he explains that a clinical study which runs during a three-year period, like many of the Gardasil studies, is largely insufficient in measuring the effect of the Gardasil vaccine on cancer or even on precancerous lesions. The criteria for comparison between the vaccinated group and the placebo group is not cancer – naturally, since cervical cancer can take anything from 10 to 20 years or more to develop and is very rare in young women. The criteria of comparison are HPV infections by one of the viruses the vaccine is aimed at and the presence of genital lesions.
Doctor de Lorgeril reminds his readers that genital lesions are generally transient and self-resolving and that only a minor percentage of these lesions will evolve into cancer.
His main point is the impossibility of measuring the effect of the vaccine on HPV related cancers and even on precancerous lesions in such a short time span. This makes sense when we remember that 90% of HPV infections resolve on their own within two years and that it can take even longer for genital lesions to appear.
With this in mind, it puts into perspective the claim that Gardasil will protect a 12-year-old child from future, hypothetical cancers.
Certainly, there is the hope of preventing future cancers, by protecting against certain HPVs associated with cancer. However, this has yet to be shown clinically.
Cancer is not the criteria for comparison in the clinical studies. It simply cannot be for the afore mentioned reasons:
- The median age for the HPV related cancers – between 50 and 80.
- Cervical cancer is a slow growing cancer that takes 10-30 years to develop.
- There is no strict causality between an HPV infection and cancer – an HPV infection is only one of several risk factors. They are self-resolving in 90% of the cases, and for the 10% remaining, if genital lesions appear, a high percentage of those also resolve on their own.
After a closer look at the numbers and the facts, we finally have a better understanding of the HPV related anogenital cancers, their frequency, their median age of occurrence, and to what extent they are detectable and treatable.
Parents need to know that:
- Cancer is a multifactorial disease, including HPV-related cancers;
- Cancer has no one singular cause;
- Cervical, anal, penile and oropharyngeal; cancers are low-incidence cancers that usually appear late in life;
- A healthy immune system is their children’s best ally when it comes to cancer;
- Screening is available and encouraged in most developed countries for early detection;
- The idea of a “magic wand” in the form of a vaccine to prevent cancer is an oversimplified way of approaching a multifaceted problem.
One might even dare ask the question – isn’t this claim of cancer prevention misleading to parents and doctors?
Another claim that is frequently put forward in media and by some doctors is that vaccinating against HPV will one day allow us to eradicate anogenital cancers associated with HPV for the younger generations.
However, when vaccinating against some of the very numerous HPV strains, other strains could potentially “take their place” and in turn become more frequently associated with cancer. Is the plan to keep adding new strains to future vaccines in an attempt to outrace nature itself? Is that why a new version of Gardasil came out in 2014?
The original Gardasil was approved in 2006 and covered four HPV strains at the time. Somehow an updated version was needed in 2014 with five additional strains.
Where do we stand after so many years of vaccinating young girls and women with one of the three different HPV vaccines?
- Gardasil,
- Cervarix, the European equivalent to America’s Gardasil, covering only two HPV strains and soon to be discontinued
- Gardasil 9
Are we any closer to “eradicating” cervical cancer?
To answer this question, we would need to compare some of the highly vaccinated countries with the countries which have a lower vaccine uptake.
America, Australia, Great Britain, Norway and Sweden are highly vaccinated countries. France and Germany not so much.
It is important to note that in many European countries a substantial decrease in cervical cancer cases and deaths started in the 80s and 90s, thanks to better screening practices. This fall began decades before any vaccine existed.
Surprisingly enough, the highly vaccinated countries do not seem to have any advantage over less vaccinated countries. Unfortunately, some of them have even started to see an uptick in cervical cancer after years of declining numbers. This is very puzzling and frankly worrying. At this point in time, it is not possible to establish a causal link between the HPV vaccination and these concerning rises in cases, however, nothing seems to suggest that the HPV vaccination has reduced numbers in any way.
These upticks in heavily vaccinated countries contradict any possible claims that vaccination could eradicate cervical cancer.
Docteur Gérard Délépine, French orthopedic surgeon and oncologist, has made use of country specific cancer statistics to illustrate this point.
USA
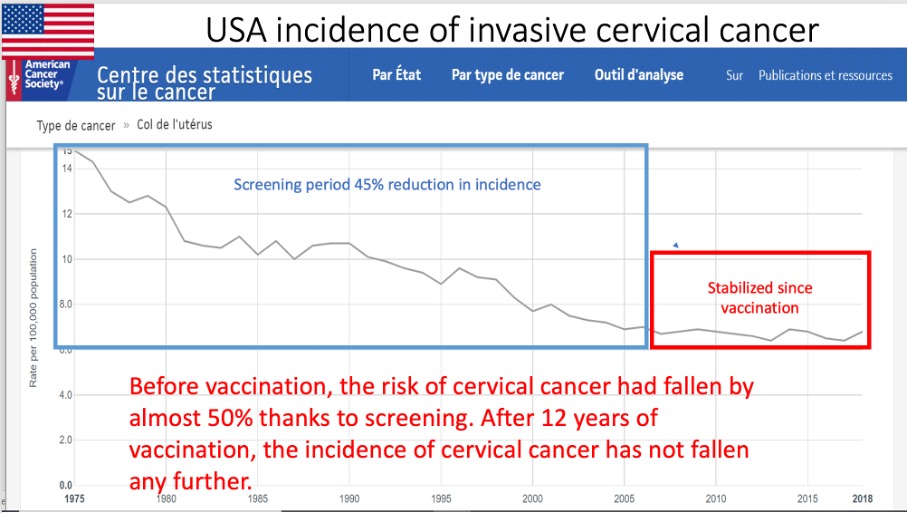
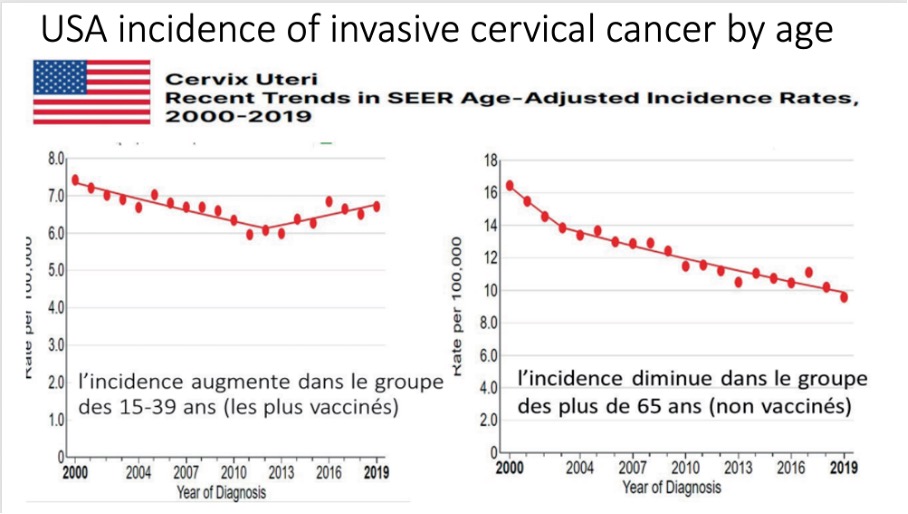
Graph 1: *Incidence increases in the 15-39 age group (the most highly vaccinated)
Graph 2: *Incidence falls in the over-65s (those not vaccinated)
AUSTRALIA
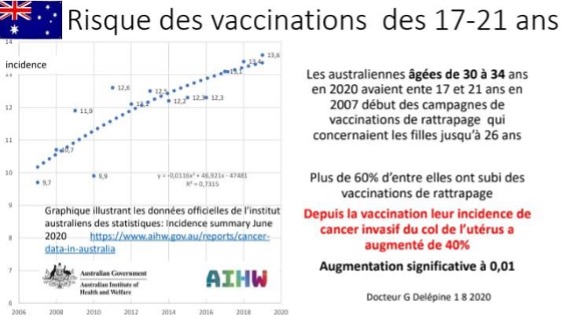
*Australian women aged 30-34 in 2020 were between 17 and 21 at the start of the 2007 vaccination campaigns, which covered girls up to the age of 26. Over 60% of them have undergone catch-up vaccinations.
Since vaccination, their incidence of invasive cervical cancer has risen by 40%. Significant increase at 0.01
GREAT BRITAIN
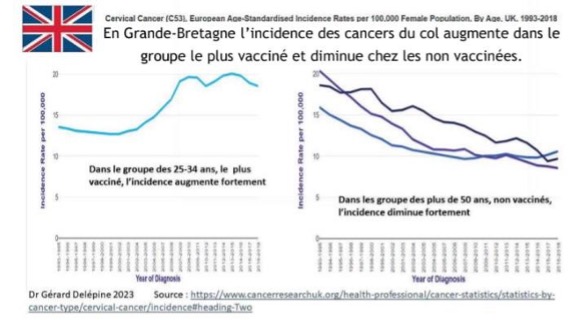
*In Great Britain, the incidence of cervical cancer increases in the most vaccinated group and decreases in the non-vaccinated group.
Graph 1: In the 25-34 age group, the most heavily vaccinated, the incidence rises sharply
Graph 2: In the non-vaccinated 50+ age group, incidence decreases sharply
NORWAY
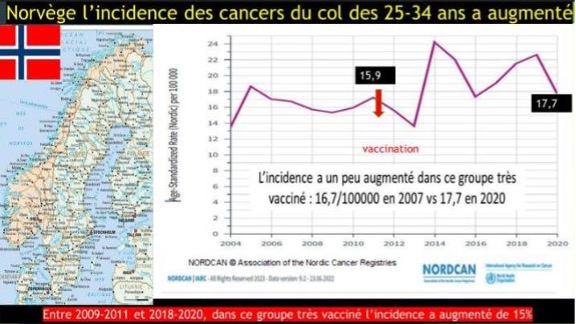
*In Norway, the incidence of cervical cancer in 25–34-year-olds has increased: 16,7/100000 in 2007 to 17,7/100000 in 2020.
Between 2009-2011 and 2018-2020, in this highly vaccinated group, the incidence increased by 15%.
As for the less vaccinated countries, he has chosen to look at two of them, Germany and France:
GERMANY
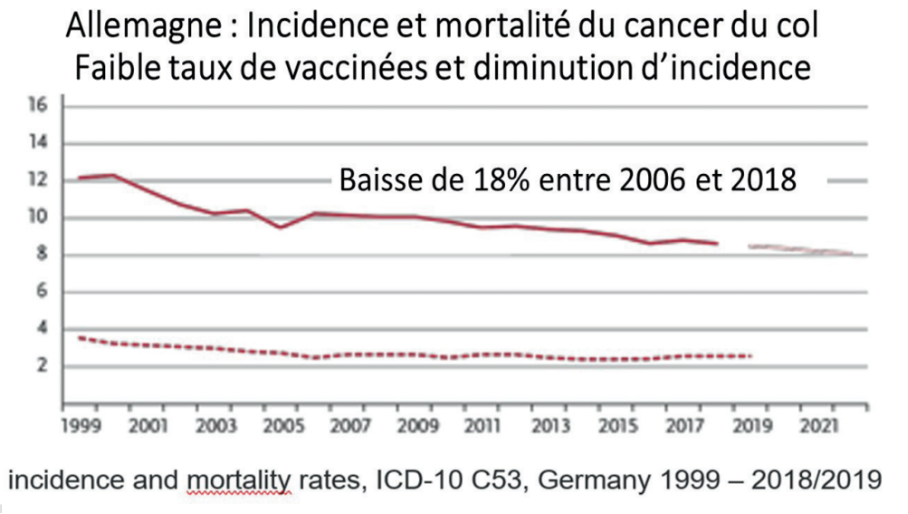
*Germany – Incidence and mortality of cervical cancer:
Low rate of vaccination and decrease in incidence.
Between 2006 and 2018 there was an 18% decrease
FRANCE
After getting a better understanding of the disease (HPV and associated cancers) and a closer look at the clinical trials as well as untangling some of the commercial “myths” attached to HPV vaccination, one last, but important question remains.
What is Gardasil’s safety profile?
All medications can cause side effects, and the frequency and severity of these side effects vary from one person to the other. This is a well-known fact in medicine.
A vaccine is given to a healthy individual, not to help alleviate symptoms or treat a disease, but in the hope of preventing future disease.
In the case of the HPV vaccine, it is given to adolescents who have practically zero risk of developing or dying from penile, anal and cervical cancer at their current age.
Without longer clinical trials it remains impossible to ascertain the vaccine’s efficacy in preventing cancer.
When you give medication to a healthy adolescent, claiming that it will help prevent a hypothetical cancer possibly 20-30 years or more into the future, the risk profile of that product needs to be practically zero.
Does the HPV vaccine have that practically flawless safety profile?
Merck claims that there is nothing special to report regarding the safety of the HPV vaccine. However, pharmacovigilance suggests otherwise.
Gardasil® is a controversial vaccine when it comes to safety, and has been since the very beginning when it was granted a fast-track approval by the FDA. The latest version of the vaccine is the 9 valent Gardasil 9 which came out in 2014. However, the first Gardasil vaccine was licensed in 2006 and covered only four strains of HPV at the time.
Thousands of reports of adverse events have appeared over the years worldwide and seem to demonstrate a plausible association between HPV vaccinations and autoimmune conditions. However, it is not easy to prove this association formally because developing and diagnosing an auto-immune condition can take years and the direct link between the vaccine and the condition can be complicated to establish.
Incriminated syndromes are orthostatic postural tachycardia syndrome, chronic fatigue syndrome, fibromyalgia, migraines or chronic headaches and the list goes on.
Gardasil on trial
While vaccination campaigns are being rolled out in Europe with claims like “eradicating cervical cancer”, “protecting your children from cancer” and the familiar “safe and effective” slogan, a multidistrict lawsuit regrouping numerous plaintiffs is being brought against Merck’s Gardasil in the United States. The plaintiffs are accusing Merck of negligence and failure to warn among other things. Merck will have to release its complete pharmacovigilance data during these trials and the cases will be tried in late 2024 or early 2025.
Children’s Health Defense (CHD) have reported on these cases on numerous occasions. Robert F. Kennedy Jr is the founder, chairman (currently on leave) and chief litigation counsel for Children’s Health Defense in the United States. In the following video clip, he takes you on a world tour exploring Gardasil’s safety track record in different countries. The excerpt is taken from CHD’s “Science Day” video, where Robert F. Kennedy Jr. walks us through some of the problems with development and safety of the Gardasil vaccine.
The stakes are very high for Merck because Gardasil is one of their blockbuster products and is becoming all the more profitable now that its indications also include boys and children of younger age groups. The fact that Europe is on board 100% in promoting the product is another golden opportunity at record profits for the pharma giant.
However, some would argue that the stakes are even higher for families. Accepting a product with a worrying safety profile for their children might work out for some, but could have far reaching consequences for others. Autoimmune conditions are for life, with varying degrees of severity. Each parent will have to consider the risk-benefit ratio for such a product individually.
The information on the Gardasil vaccine conveyed by public health institutions, both nationally and internationally, mostly parrot the claims of the vaccine manufacturer. This is not where you can find a critical scientific analysis of the existing studies and data. Looking at pharmacovigilance data will offer some information on the types of injuries, but there is always the bias of underreporting. This is why it is essential to seek out independent, unbiased information from multiple sources.
What to ask your doctor?
Interesting questions to ask your doctor are:
- Are you familiar with the European medicines agency’s assessment report on the Gardasil 9 vaccine?
- What can you tell me about the side effects mentioned in that document?
- Are there ingredients I should be worried about in terms of allergies?
- Has the toxicity of the adjuvants been studied in separate clinical trials?
These are basic questions which many doctors cannot answer. However, if they recommend a product, one expects them to be able to answer in-depth questions about it. Ultimately, they are supposed to help a parent weigh the risks and benefits for their child when using a medical product.
Thankfully, responsible doctors do exist. They go that extra mile to expand their expertise and will not stay focused merely on the possible benefits, but also explain the risks, when proposing a product.
For parents who would like to do their own research, there are several informative books written by independent researchers about the Gardasil vaccine and its clinical trials. They are accessible to the public and the graphs and information given are thoroughly explained and simplified for parents and doctors. A very accessible one is Doctor De Lorgeril’s book “les Vaccins contre les cancers…”
Another book worth reading is written by two French oncologists, Doctor Nicole Délépine and Doctor Gérard Délépine. Their book, “Gardasil – Faith and Propaganda versus hard evidence” has been translated into English and specifically addresses the Gardasil vaccine.
EMA’s assessment report on Gardasil 9
The European Medicines Agency’s (EMA) 128-page assessment report on the Gardasil 9 is also valuable, but slightly more challenging to read. The document contains an enormous amount of information. The data on adverse events during the clinical trials start on page 112 and is exposed in the following pages.
The report goes through injection-site adverse events (swelling, pain and erythema – very common), systemic adverse events (commonly headache, pyrexia and nausea with this vaccine) and then the serious adverse events that occurred during the clinical trials:
“A total of 23,266 subjects were vaccinated in 7 clinical trials. A total of 15,776 subjects received at least 1 dose of 9vHPV (Gardasil 9) vaccine, and 7391 subjects received at least 1 dose of qHPV (the previous Gardasil) vaccine…”
“There were a number of serious adverse events (SAEs) occurring in the clinical trial program which are considered adverse events of special interest or are related to previously identified safety concerns: ulcerative colitis, Crohn’s disease, multiple sclerosis (2 events), sarcoidosis, intracranial venous thrombosis, deep venous thrombosis, syncope (5 events), and orthostatic hypotension. Upon review these do not raise any new safety concerns. The occurrence of cases of POTS, CRPS, pulmonary vasculitis, and leukaemia are discussed separately below.”
In addition to the serious adverse events, seven deaths have occurred. They are mentioned, but considered unrelated to the vaccine without specifying the exact reason for this:
“A total of 5 subjects administered 9vHPV vaccine died during the entire study period. Two additional cases have been reported after the data cut-off in the original application. None of the deaths were considered related to the 9vHPV vaccine.”
As for the additional discussion around the leukaemia cases, the report goes on to mention five cases of acute leukaemia. This number exceeds “the expected number of cases”, however this is not considered sufficient to implicate a causal relation between the vaccine and the disease.
“Five cases (4 with 9vHPV and 1 with qHPV) of acute leukaemia have been reported, three in subjects younger than 20 years of age at diagnosis. While the observed number of cases of leukaemia exceeded the expected number of cases, this is based on a few observed cases in relation to a very low background risk for leukaemia in this age group. Such a comparison will inevitably be sensitive to random occurrences of single cases and is not considered sufficient to implicate a causal relation in this case.”
What seems rather striking in the report, is the “difficulty” of establishing a causal relationship between a side effect and the vaccine. A side effect is “unrelated”, “insufficient” or “do not raise concern” in most cases. The benefit of the doubt is for the vaccine and not the future patient.
On the contrary, it is not “difficult” at all to infer vaccine efficacy. In this area, there is a lot of goodwill and optimism, even when firm proof is lacking.
“Considering that it is not possible to investigate efficacy in boys or girls 9-15 years of age due to sexual naivety, the agreed strategy to demonstrate the efficacy of the vaccine was to generate efficacy data in 16-26 years old women and to extrapolate this data to younger subjects based on immunogenicity (bridging) data. This approach was already proved valuable for previously authorised HPV vaccines.”
“Thus, it can be concluded that the 9vHPV is highly likely to protect girls 9-15 years of age against the 9 HPV types included in the vaccine and also to protect boys 9-15 years of age against relevant endpoints.”
Vaccine efficacy is “highly likely” and data from a different age group can be “extrapolated” to a younger age group. What they call “serological bridging to the efficacy population” has been accepted as a surrogate for demonstration of protection in another target population.
However, the report clearly states that the duration of the vaccine induced protection is uncertain:
“To date, persistence of antibody response induced by the 9vHPV vaccine was demonstrated for up to 3.5 years in women 16-26 years old (study 001), with waning immunity noted for each vaccine type. In subjects 9-15 years of age, immunogenicity follow-up is available for up to 3 years after vaccination with similar results. With respect to the clinical program, neither efficacy nor immunogenicity of Gardasil 9 was assessed in women older than 26 years of age”.
This confirms Doctor De Lorgeril’s statements from his book. The clinical trials do not exceed 3 years in duration, and this makes them incomplete in demonstrating protection against cancer and precancerous lesions. It is also unknown for how long immunity will last since waning immunity was noted during the trials. Let’s also keep in mind that the larger part of the cancers in question have a median age of occurrence closer to 60 or 70 years of age, and that cervical cancer is a very rare occurrence before age 26.
The report adds:
The Committee for medicinal products for human use (CHMP) therefore “considers the following measures necessary to further confirm the efficacy of the Gardasil 9:
· long term follow up studies to monitor long-term effectiveness and immunogenicity of 9vHPV vaccine and to obtain information on duration of effect in women and adolescents 9-26 years of age.
· A post-marketing immunogenicity and safety study of the 9vHPV vaccine in women 27 to 45 years of age.”
The Committee for Medicinal Products for Human Use (CHMP) is asking Merck to proceed with further studies to confirm the efficacy of their product. It is work in progress. The current state of knowledge of the product is susceptible to evolve in the years to come.
It’s also worth noting that Gardasil 9 has not gone through genotoxicity nor carcinogenicity studies. Genotoxicity studies are needed to know whether or not the medicine can lead to damage or mutations in the human DNA and carcinogenicity studies whether the medication can induce or aggravate cancer.
The EMA assessment report confirms that the Gardasil’s genotoxicity and carcinogenicity have not been evaluated. This could be worrying to a parent when considering the HPV vaccination. When vaccinating your child in the hope of preventing future cancers, one would naturally like to be sure that the product in question will not induce cancer. This seems to be essential information in considering the safety of a product.
As with most medicinal products, surveillance and long term, post-marketing studies are required. Science is always a continuum of knowledge and requires time and experience in order for conclusions to be reached. The fact that a product is put on the market, does not mean that everything is known about it. With the Gardasil 9 many questions remain, the science is not settled. The EMA assessment report confirms this. Unfortunately this point is not stressed when campaigns to increase vaccine uptake are launched.
An advertising campaign is merely a still picture in time, representing a small piece of a more complex and even distorted reality. It will always highlight possible benefits, without dwelling on risks. This is only to be expected when one considers the enormous financial interests that do exist behind such campaigns. This point is important to keep in mind.
TAKE YOUR TIME
Take the time to do your own research into medical products you are planning to use.
- How severe is the disease? How frequent is it?
- Is it treatable if detected in time?
- Is the treatment necessary or are there other alternatives?
- Is it a safe and effective product? Does it have a good track record? What are its side effects?
Read the package insert thoroughly and visit your country’s pharmacovigilance website or Eudravigilance for European numbers.
Look at the list of ingredients and make sure you understand the action they will have in the body.
Just as you might read customer reviews and technical information when purchasing a new car in order to make the right choices for you, a similar approach can be beneficial when reflecting upon medicines you or your children are considering. No one would find it surprising if you read the ingredients’ list on the food you purchase or the shampoo you use. Why would we be any less careful with the medicines and vaccines we put in our bodies or our children’s bodies?
Never rush when making health decisions for yourself and your family.
Watch our HPV Vaccine Exposé below to get informed
For those who would like to dive deeper into the stories of those who initially rushed to get the Gardasil vaccine and who then experienced serious, life-changing side effects from it, these books are available in English:
It is also possible to read the stories of some of the many plaintiffs in the ongoing multi-district lawsuit against Merck here. Children’s Health Defense (The Defender) has published articles for several years relating their stories to the public. Many of them exist in multiple languages:
Sahara Walker Michael Colbath, Kayla Carrillo, Korrine Herlth, Savannah Flores, Abigail Stratton, Zachariah Otto, Julia Balasco, Emma Sullivan, Merrick Brunker, Victoria Trevisan, Catherine Boss, Kaley Stockton, Caroline Cantera as well as Christina Tarsell (died 18 days after her third Gardasil shot) and Noah Tate Foley (died after developing numerous health issues after his first shot of Gardasil).
Suggest a correction