Herd Immunity: Science Or Magic?
What trick is being used to try to get the world’s population to accept compulsory vaccination, and give up fundamental freedoms? Undoubtedly, it is the argument of the threat to public health, with the great return of epidemics and the unique solution to be protected against them: vaccination coverage. This vaccination policy, which promises a triumph over germs, is based on the sacrosanct ‘herd immunity’, a concept presented as a certainty, but which might actually be no more than an illusion.
The magic of herd immunity
In August 2014, William Thompson, an expert from the CDC, confessed that he had been pushed by his superiors to manipulate studies on the possible link between autism and the MMR (measles-mumps-rubella) vaccine. A few weeks later, the first meeting of the Global Health Security Agenda (GHSA) orchestrated by the WHO at the White House set a goal of mandatory immunization on a global scale with a target of 90% immunization coverage rate (now increased to 95%) for this same vaccine.
 From January 2015, the measles epidemic at Disneyland in California is then used as a pretext for an unprecedented media hype. The threat is serious. “Measles is on the march”, American television stations announce the number of reported cases every day with great fanfare. Soon after this, the new bill SB277 puts an end to exemptions for personal and religious reasons, forcing many parents to withdraw their children from public education. Non-vaccinated people are now being blamed and tracked, as they would endanger others by not contributing to the herd immunity and would undermine the goal of eradicating the disease.
From January 2015, the measles epidemic at Disneyland in California is then used as a pretext for an unprecedented media hype. The threat is serious. “Measles is on the march”, American television stations announce the number of reported cases every day with great fanfare. Soon after this, the new bill SB277 puts an end to exemptions for personal and religious reasons, forcing many parents to withdraw their children from public education. Non-vaccinated people are now being blamed and tracked, as they would endanger others by not contributing to the herd immunity and would undermine the goal of eradicating the disease.
In retrospect, nothing in this episode, that seemed tailor-made to promote measles vaccination, genuinely argues in its favor. Most of the children who contracted measles at Disney had received two doses of the vaccine and, shockingly, 38% of the cases were even found to be infected with a vaccine strain!
By the end of 2019, still not a word about these ‘later findings’. Mickey’s magic is still operating, promoting herd immunity and vaccination coverage. Last October, Arthur Caplan, the director of New York University’s medical ethics section, re-launched the campaign by declaring that “bringing an unvaccinated child to Disneyland is an immoral and selfish act to do”. And while there were less than hundred cases of measles in California for the whole year (and no death), another draconian bill just passed. It now restricts contraindication certificates to vaccination and introduces controls that will cost the administration nearly $10 million a year. But it seems immunization coverage must be achieved at all costs.
If the ‘Mickey Mouse magic’ is pointed at here, it is because, beyond a touch of irony, one can doubt if the very notion of a ‘herd immunity achieved through vaccination’ really is a solid scientific concept. Is it really a coincidence that, at the Global Vaccination Summit recently held in Brussels with the WHO and the European Commission, one of the three topics discussed was entitled ‘The Magic of Science‘?
The take of the media
Although politicians and experts constantly refer to it, reminding us that it is a goal set by the WHO, it is usually the journalists who generally are at task to explain the concept of herd immunity.
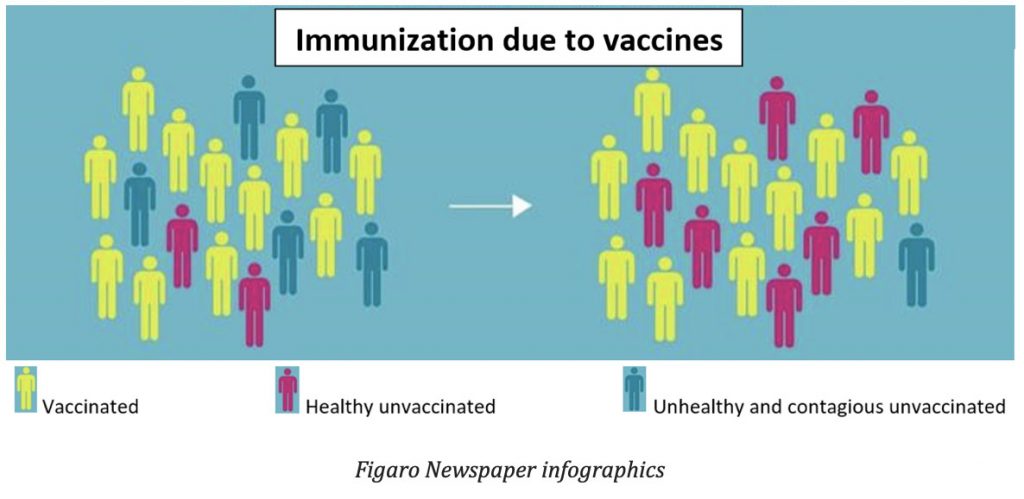
For example, in the French TV programme “Toc Toc Docteur” broadcast on a main channel before the vote on 11 compulsory vaccines in France, it was the health journalist from Le Figaro newspaper, sitting next to Professor Daniel Floret, who stressed the importance of achieving high vaccination coverage: “This will make it possible to interrupt the transmission of a virus or bacteria in a population, as long as a sufficient percentage of individuals are immunized against the disease”. “Above a certain threshold of vaccination coverage, the disease cannot be maintained in the population and eventually disappears,” he adds. He goes on to mention the eradication of smallpox as an example of the success of this vaccination policy (whereas in reality it is not vaccination, but the detection and isolation of patients and their contacts that has overcome the disease, as can be seen in the WHO’s final eradication report and in interviews with Donald Henderson, the senior official in charge of this operation – see The global eradication of smallpox : final report of the Global Commission for the Certification of Smallpox Eradication, Geneva, December 1979, p. 32. Bibliothèque en ligne de l’OMS // « Smallpox : dispelling the myths. An interview with Donald Henderson » Bulletin of the World Health Organization, vol. 86 : 2008, num. 12 , 909-988).
Figaro Newspaper infographics
The critical viewer would have noticed that it was the journalist preaching the promise of this vaccine miracle and not the professor, whose tacit presence was supposed to confer a ‘scientific validation’ to his words. Indeed, the latter was very well aware that in order to eradicate the disease, it would be necessary, at the very least, that vaccination be effective for all, throughout life, and that it blocks the transmission of the virus. But since the experts know that these assumptions are currently all being thwarted and discussed in scientific articles and conferences, it is logical that they remain silent on air.
The take of science
Surprisingly, there is no real consensus on what determines herd immunity, let alone how it is calculated. A review article on the history, theory, and practice of herd immunity, written with input from the CDC, provides an eloquent illustration of this. The author, Paul Fine, introduces it as follows:
“The concept has a particular aura in that it implies an extension of the protection afforded by a vaccination program from the vaccinated to the unvaccinated, as well as an apparent provision of means aimed at the total elimination of certain infectious diseases” (P.Fine “Herd Immunity: History, Theory, Practice” Oxford Journals of Epidemiologic Reviews, vol. 15, n°2, 1993, p 265-301). The use of words such as ‘aura’, ‘apparent provision‘ and further in the text ‘the magic of herd immunity‘ is interesting here too, as it shows the vagueness surrounding the concept and its associated mechanisms.
Historically, the notion of herd immunity, derives from observations around the fact that in some diseases, epidemics end when a given threshold of sick people is reached, apparently leaving part of the population unscathed.
Initially, the interpretation of these facts had given rise to violent controversy. For some, it was related to changes in the properties of the infectious agent (e.g. decrease in the virulence of the pathogen as it passes from one host to another), while for others it was the result of a dynamic between the pool of people likely to be infected and those with immunity acquired by the disease. Each camp also supported its thesis with mathematical reasoning, but the second group prevailed, and supported its theories with a simple mathematical formulation (subsequently revised) related to the ‘principle of action of the mass’ introduced by Hamer in 1906 (Hamer WH. Epidemic disease in England—the evidence of variability and of persistency of type. Lancet 1906; 1:733-9).
In 1930, a publication by Dr. Hedrich gave the first notorious illustration of the term ‘herd immunity‘. The term then referred to natural immunity in a defined population, acquired by a group of people who had developed the disease. After collecting epidemiological data on measles over a 30-year period, Hedrich observed that epidemics occurred when the proportion of children under 15 years of age at risk of developing the disease approached 50% and that, when epidemics stopped, there was always a pool left estimated 32% … At the same time, Hedrich also noticed that more than 95% of children had had measles at this age, having faced successive waves of epidemics (Hedrich AW. “Monthly estimates of the child population susceptible to measles, 1900-1931, Baltimore, MD.” Am J Epidemiol 17, 613-636 (1933)).
Later in the 1960s, when the first measles vaccines were developed in the USA, it was assumed that the immunity induced by a vaccine would be equivalent to that created by the disease, so much so that the word ‘vaccination’ was soon replaced by the word ‘immunization’, a confusion of vocabulary that bears serious consequences. Based on this belief, and Hedrich’s observations, the American health authorities went so far as to imagine that it would take no more than a year of mass vaccination to achieve measles eradication (Sencer DJ, Dull HB, Langmuir AD. Epidemio- logic basis for eradication of measles in 1967. Public Health Rep 1967;82:253-6).
But while vaccination campaigns have contributed to a drastic reduction in the incidence of the disease in its clinical form, the promise of eradication remains a failure and recurring epidemics are turning the expected miracle into a mirage that is endlessly drifting further away. Many factors related to the complexity of the immune system and its interaction with its environment seem to permanently compromise this ideal.
‘Variable’ vaccine efficacy
The fact that some vaccines can induce some degree of immunity and reduce the incidence of certain diseases is indisputable. In the case of live virus vaccines (e.g. measles, mumps, rubella, varicella), which are those for which the benefit of herd immunity is generally claimed, the subject is actually infected with the virus, but in an attenuated form. The host then develops an asymptomatic infection, which is considered both ‘non-communicable’ and ‘inducing a sustained immune response’. The challenge is therefore to induce an ‘effective’ response, i.e. a lasting memory of the disease while not causing any symptoms or infecting other people. If science once considered this possible, evidence shows that this postulate is now collapsing.
Vaccination primary failure
Official sources generally claim that the rate of efficacy is over 90% for the measles vaccine, taking into account that there are between 2 and 10% of ‘non-responders’, in whom the vaccine has no efficacy. The reasons are probably genetic, although they have not yet clearly been identified.
But what is not said is that for responders, efficacy is variable. As a doctoral thesis on the subject states, “the immunity acquired by the measles vaccine appears to be a continuum, ranging from full protection to minimal or no protection, to partial or temporary protection. This flexibility of the immune response is responsible for the occult circulation of the virus in the vaccinated population.” (Diane Ninkam Nghemning “Souches africaines du virus de la rougeole : étude de l’interaction virus-cellule et analyses phylogénétiques” thèse doctorale en faculté de biologie à l’Université J. Fourier, Grenoble 1, 9 juillet 2002).
As an example, an antibody level of 120 mlU/ml is assumed to be immunizing against measles, and enough to declare the vaccine ‘effective’. But recent studies have prompted reservations on these figures. A Chinese study, designed to determine actual levels of protection, estimates that nearly 1000 mlU/ml, a value almost ten times higher, is needed to prevent not only the development of symptoms, but also transmission of the virus (Lee, Min-Shi & Nokes, david & Hsu, Hsu‐Mei & Lu, Chih‐Feng. (2000). Protective titres of measles neutralising antibody. Journal of medical virology. 62. 511-7). The study estimates that levels between 120 and 500 mlU/ml prevent the clinical development of disease, but not the propagation of the microbe. Previously a team of American experts had already reached similar conclusions.
Failure in infants
This is certainly one of the biggest pitfalls of vaccination. Infants whose immune systems are not yet developed at birth are normally protected by antibodies transmitted by their mothers during pregnancy and breastfeeding. When a mother had the disease, these levels were high enough to protect the baby until 12 or 18 months of age. Unfortunately, due to the introduction of vaccination, the antibodies transmitted are no longer sufficient, and infants are at much higher risk than before (J. Lennon, F. Black, “Maternally Derived Measles Immunity in Era of Vaccine-Protected Mothers”, Journal of Pediatrics, 1986 May, 108, 671-6). Vaccinating early is not the answer, as the vaccine is somehow neutralized by the presence of maternal antibodies and protective levels are different from one individual to another.
The consequences of this problem are particularly worrying. This is evidenced by the fact that the incidence of disease and mortality in children under 2 years of age is currently increasing in all countries where measles is circulating (Rapport sur les épidémies de variole en France, BEH n°33-34 du 20 septembre 2011, p. 356.W. Moss, P. Strebel). An additional consequence of this phenomenon is that it creates a natural reservoir of virus so that ‘eradication’ virtually becomes impossible to achieve.
Vaccination secondary failure
This is the decrease in antibody levels over time in those who have been vaccinated, making those supposedly protected vulnerable again. This phenomenon is well known to scientists, but rarely acknowledged in official speeches. It is estimated that on average this decline in antibodies takes place over a period of about 7 years, but several recent studies suggest that vaccine immunity could disappear much faster.
According to data provided by Physicians for Informed Consent (see table at end of article and download pdf) an american doctors association, 35% of 7 years-old children have antibody levels below 900 mlU/mL and are likely to develop asymptomatic measles. This figure rises to 60% after the age of 15.
Wherever it circulates, epidemiological data show that the disease is now affecting vaccinated young adults in whom antibody levels are no longer sufficient to prevent the development of the disease.
In Europe, official statistics for October 2019 from the European Centre For Diseases Control show that there were approximately 12,000 cases of measles in Europe, 29% of whom being children under 5 years and 55% of whom were over 15 years old. The category with the highest incidence are children under one year of age with an average of 281 cases per million.
Overall, of the cases whose immunization status could be verified, 29% had been vaccinated. It is worrying that the ECDC report only recommends greater immunization coverage, without addressing the problem of risk shifting to the most vulnerable age groups, or proposing complementary or alternative solutions.
The silent circulation of viruses
The variability in individual response to the vaccine in terms of seroconversion (the level of antibodies in the blood) and the decrease in vaccine efficacy largely explains the ‘silent circulation’ of vaccine viruses.
The vaccination campaign in Greenland (I. Pedersen, H. von Magnus, “Subclinical Infections in Vaccinated Seropositive Individuals in Arctic Greenland”, Vaccine, Vol. 7, Issue 4, Aug. 1989, p. 345-348), where more than 90% of a ‘virgin’ population (where the disease did not exist) was vaccinated, has produced results that confirm this phenomenon. A check of the antibodies 2 to 4 years after vaccination showed a high increase in antibodies in about 63% of the subjects, indicating that they had therefore been infected with the vaccine virus circulating ‘quietly’, i.e. without any clinical symptoms. With two-thirds of those vaccinated affected, this episode can be considered a true ‘silent epidemic’ spread by the vaccine virus.
In addition, a very recent study reports the persistence of the vaccine strain in its host up to 100 or even 800 days after vaccination (J. MacMahon, I. Mackay, S. Lambert “Measles Vaccine Virus RNA in Children more than 100 Days After Vaccination”, Viruses, 10 July 2019). This could imply a possibility of transmission by vaccinated subjects that extends well beyond the 2 to 3 weeks sometimes mentioned.

Strain Substitution
There are still other problems with these vaccination policies. The Pasteurian model, and that of vaccination in general, is challenged by the complexity of the microbial ecosystem, and frequently another strain of the same infectious agent replaces the strain of the vaccine. This is well known for other diseases, and the pharmaceutical industry has embarked on a race to chase the viruses, in an attempt to identify and incorporate the new dominant strains into their vaccines.
For example, after the introduction of the pneumococcal vaccine Prevenar 7, the incidence of pneumonia increased. A new vaccine, Prevenar 13, has therefore incorporated six additional strains but a Prevenar 20 is now in development. The same phenomenon occurs with other vaccines, such as the anti-HPV Gardasil 4, which is gradually being replaced by Gardasil 9. The measles virus also seems to be following the same trend and this could mean a much more serious problem, since it is a much more contagious disease.
The original ‘antigenic’ sin
In the case of vaccine resistant strains, vaccination may even have an adverse effect due to the primary immune response. This is because the body keeps a memory of the first infections or vaccinations encountered and against which it had to develop antibodies. Consequently, if other infections or related strains subsequently infect the body, it will react less intensely to them, as its cellular memory remains largely focused on the primary infections, even if these microbes have disappeared from the body.
This mechanism related to ‘primary infection’ could explain many vaccination failures, such as pertussis. Recent epidemics in the United States have resulted in a higher incidence rate among those who have received multiple doses of vaccine than among those who have not been vaccinated (one article reports that one private school had 50% of its students who had pertussis, even though they were ALL vaccinated – S. Attkison “Whooping Cough Outbreaks Amongst Vaccinated in California: LA Times”, sherylattkison.com, 29 Oct. 2019). The health authorities were forced to admit that they had ‘misunderstood the immunity induced by this vaccine’. Unfortunately, children vaccinated with an acellular pertussis vaccine will now remain more likely than others to contract the disease again for the rest of their lives! (J. Cherry, “The 112-Year Odyssey of Pertussis and Pertussis VAccines. Mistakes Made and Implications for the Future.” J Pediatric Infect Dis Soc. 2019 Sep 25;8(4):334-341. doi: 10.1093/jpids/piz005)
If a similar phenomenon were to occur for measles, revaccination would be tantamount to weakening the population. It could even lead to a situation similar to that of ‘virgin’ populations, i.e. as vulnerable as if they had never encountered the virus (A. Wakefield, “The Sixth Extinction: Vaccine Immunity and Measles Mutants in A Virgin Soil”, Journal of American Physicians and Surgeons, Vol. 24, n°3, Fall 2019, p. 72-794).
Epidemics of mutants
As with antibiotic resistance, selection pressure on the strains used for the vaccine can lead to the emergence of new strains resistant to the vaccine. In recent measles epidemics, ‘mutant’ strains have been identified that escape the neutralization of antibodies generated by the measles vaccine. These new genotypes e.g. H1, D4, D8, and B3, are spreading worldwide and affect vaccinated people (vaccines use type A strains). In a recent article, the French Professor Didier Raoult, one of Europe’s most respected and published infectiologists, draws attention to the B3 strain, which is described as more transmissible and more pathogenic. According to him, “The consequences of the emergence of this new B3 strain on the effectiveness of the current vaccine regimen and on the goal of eradication are unknown.”
In spite of this serious warning, media and our health authorities have kept completely silent about this danger. It is also worrying that the video he recorded on the new measles outbreaks has disappeared from his station. The video clearly mentioned the limits of measles vaccination, citing the example of China and Mongolia, two countries that practice compulsory vaccination with maximum coverage (between 97 and 99%) with two or sometimes even three doses.
In Mongolia, where immunization coverage has been above 95% since 2015, the elimination, declared in 2014, was followed by a resurgence of the disease a few months later, and an epidemic of more than 57,000 cases, causing 147 deaths, mainly among children under one year of age.
Impossible to eliminate
The question is not new. In 2012, Gregory Poland, a world expert who heads the journal Vaccine, was already paving the way in an article on measles vaccines: “The question remains open as to whether the current vaccines are effective enough to eradicate the disease, even considering that measles can be controlled and eliminated in some areas over a period of time. In reality, there is no way of knowing whether elimination can actually be achieved and maintained”. »
As Professor Raoult makes clear, the problem is complex. The solution is not simply to vaccinate with three or more doses (the increase in antibodies then drops in a year), and there is no guarantee that if a vaccine is developed ‘urgently’ with these new strains, the virus will not mutate again.
Measles, the worst-case scenario?
Without mentioning the situation of the new strains, taking into account the various factors mentioned above, according to Levy’s projections, in a few decades (around 2050), the percentage of vaccinated people likely to be affected by the disease would exceed the percentage of susceptibles that existed before the era of vaccination. (so vaccination could actually destroy the herd immunity that had been created by decades of exposure to measles)
A study, this time conducted by Heffernan in 2009 (JM Heffernan, “Implications of Vaccines and Waning Immunity”, Proc. Biol. Sci. ,2009 June 7, 276, 2071-2080), predicts that with a high vaccination rate (above 80%), taking into account the decrease in vaccine efficacy (up to 30 years), cycles of large-scale epidemics are to be expected. It estimates that these massive epidemics should start to occur about 52 years after the start of vaccination programs, i.e. as far as we are concerned within 3 to 10 years!
Could the situation develop into a worst-case scenario?
While health authorities continue to hammer home the myth of herd immunity, one of the vaccination popes has recently made an amazing confession about the failure of measles vaccination. Last November, Dr Stanley Plotkin, who has developed many vaccines and is the author of ‘Vaccines’, the book considered to be the ‘bible’ in vaccinology, wrote a comment entitled “Is There a Correlate For Protection in Measles Vaccine”, a title that could be translated into common language as “Do Measles Vaccines Work?”. Analyzing current epidemics, the article clearly attributes the failure of vaccination to the error in estimating the level of antibodies needed to block transmission (silent circulation of the virus among the vaccinated) and to the emergence of new virus strains of type H1, D8 or B3. Why is it that the most prominent advocate of vaccination is now making such an admission? Is this a warning in the face of an explosion of measles cases? Is it a simple desire to maintain scientific credibility? Is it a refusal to participate in a lie that could lead a whole population into a totalitarian scenario? Or, on the contrary, a pretext to outbid and re-vaccinate the entire population?
For the time being, it would be advisable, first and foremost, to exorcise the population from the fear of infectious diseases that is constantly being instilled. It is time to address the real health threats that afflicts our society, the explosion of chronic, autoimmune, inflammatory and neurodegenerative diseases.
Even if we are witnessing major measles epidemics, solutions can surely be put in place (e.g. taking vitamin A, isolating patients, home visits etc.) and, all things considered, measles remains a benign disease.
Right now, lifting the veil on the magic that surrounds the notion of herd immunity is of critical importance for the sake of health and democracy around the globe.
What if…Vaccine ‘Herd Immunity’ is an illusion.
How big is the real ‘herd?
- Estimate of the ‘real herd’ in France
In a scenario that excludes real life immunity acquired from the disease, taking into account the factors that contribute to measles vaccination failure, the population with a strong immune status acquired through vaccination would be around 30%. Can herd immunity really be achieved through ‘vaccination coverage’?
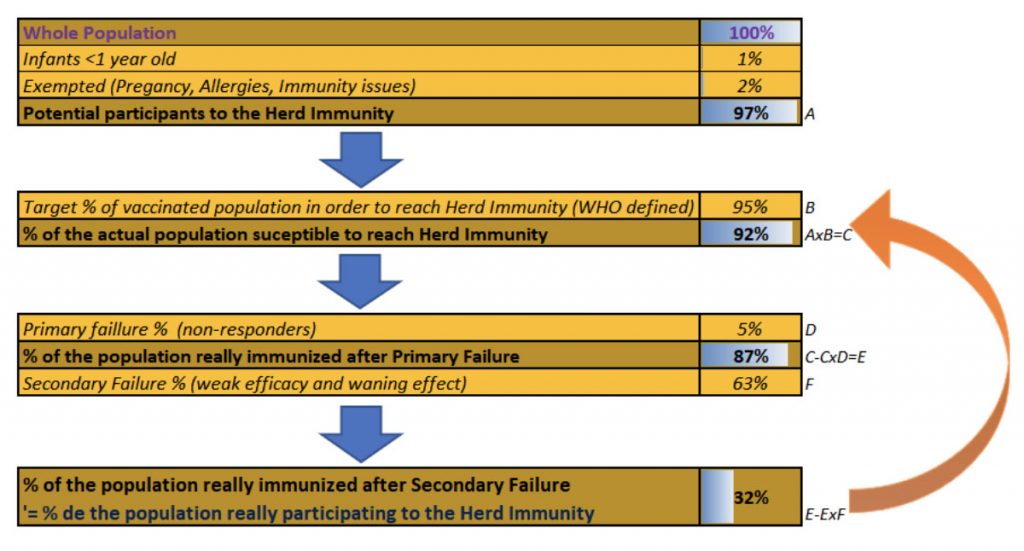
After excluding at-risk people who cannot be vaccinated, 97% of the population remains for ‘the herd’. If 95% of the population is vaccinated (according to the vaccine coverage target for achieving herd immunity), 92% of the population is actually vaccinated. Of this group, 5% are non-responders (who develop almost no antibodies). This leaves 87% who are expected to be fully protected in order to achieve herd immunity. If 63% of these fail due to an immediate response insufficient to block transmission of the virus and/or a rapid decrease in the efficacy of the vaccine, only 32% of the population is actually participating in herd immunity.
In reality, taking into account the fact that the percentage of the population that truly had the disease (57% were born before 1983, the year of introduction of the vaccine into the calendar) is steadily decreasing, the objectives of eliminating measles through vaccination coverage seem seriously compromised.
Originally published on Nexus.fr
Suggest a correction